Your 4 Questions About Plantar Fasciitis Answered!
Your 4 Questions About Plantar Fasciitis Answered!
What is the plantar fascia anyways?
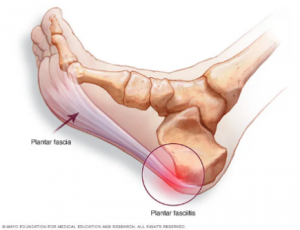
Plantar fascia is a thick band of tissue running along the bottom of your foot extending from your heel to the base of the toes. This band of tissue helps to propel you forward when you walk and run. You also have multiple muscles that attach to and/or cross the plantar fascia.
So what is plantar fasciitis?
Plantar fasciitis is when the plantar fascia becomes inflamed and can be very painful with walking, standing, and running. Plantar fascia can have many causes and the pain can vary from very severe, sharp pain, to a less intense, achy pain. Usually there is a significant and sudden change in your activity level that will give rise to inflammation of the plantar fascia, such as starting a new walking routine or increasing the mileage of your walking/running routine too quickly.
How do I know if I have plantar fasciitis?
If you have pain around the bottom of your heel, arch, or around the base of the toes along the bottom of your foot this could be indicative of plantar fasciitis. You may also have tightness through your calf muscles and/or your big toe. Do you have pain in your feet when you take your first few steps after getting out of bed in the morning which resolves at least somewhat with walking around? Do you also have pain with prolonged standing and walking? These factors can all be indicative of plantar fasciitis, but you should go see a Doctor of Physical Therapy at Live to Move to determine if you have it and could benefit from therapy.
How can physical therapy help?
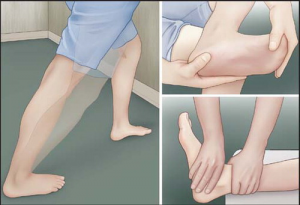
A physical therapist can assess you for the root cause of your pain through reviewing your history and performing a physical exam. Your physical therapist will then write a plan of care to determine how much therapy you may need. Your treatment sessions will likely include a combination of manual therapy to get the joints and soft tissues moving optimally, as well as strengthening and stretching of the ankle, knee, and hip muscles to address any muscles imbalances. You will also receive education regarding any activity modifications you should make with your daily activities. (You can also ask about dry needling which is another tool used at physical therapy to address your pain and get you back to your activities as quickly as possible!)
Don’t let plantar fasciitis hold you back any longer. Contact Live To Move Physical Therapy today to schedule your consultation and start your journey toward a pain-free, active life. Your feet—and your future self—will thank you!
Other
COMMENTS: No Comments
What is Pain and Why do I Have it?
What exactly is pain?
Pain is a multi-dimensional phenomena affected by many internal and external factors. The purpose of pain is to warn the body of tissue damage OR the threat of potential tissue damage. You may have pain because you recently sprained your ankle, or you may have pain from an old back injury long after the injured tissues have healed. In both cases pain is present, but only in one case is there current tissue damage. When you experience pain, the brain is trying to warn the body of a perceived threat which may or may not actually be threatening. Regardless, pain is pain.
Why do I have pain?
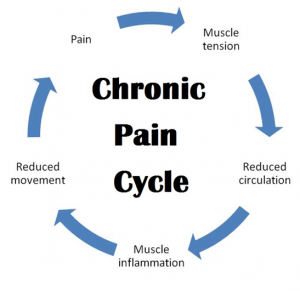
You may be someone with appropriately regulated pain which subsides as the tissue heals. Or you may be someone with acute pain that extends past the point of tissue healing, which is considered chronic pain. This is when the brain’s pain modulation system is no longer working as it is intended. A lot of people in this category have had multiple experiences with pain in the same area or multiple areas of the body sensitizing the brain to pain. This further leads to a cycle of decreased sleep, activity, and overall brain function making it difficult for your pain modulation system to restore itself. You can break this cycle over time by restoring general brain health through nutrition, exercise, sleep, and even something as simple as prioritizing things in your life that make you happy.
According to the CDC, in 2019, 20.4% of adults had chronic pain and 7.4% of adults had chronic pain that frequently limited life or work activities
How can physical therapy help?
The cycle of chronic pain CAN be broken, and Physical Therapy can help you with this process. Whether you have low back pain, chronic headaches, or widespread pain, our Doctors of Physical Therapy can help you with physical rehabilitation as well as helping restore your brain’s pain modulation system. This is achieved through strengthening, improving neurovascular health, and pain neuroscience education.
Physical Therapy can help you to overcome your pain and return to participating in the things you love!

(Google trend related queries: COVID, back pain, neck pain, chronic fatigue syndrome, chronic elbow pain, elbow pain, pelvic pain, ankle pain, what is chronic pain, chronic pain syndrome
Other
COMMENTS: No Comments
What to Know About Spondylosis
What does Spondylosis mean?
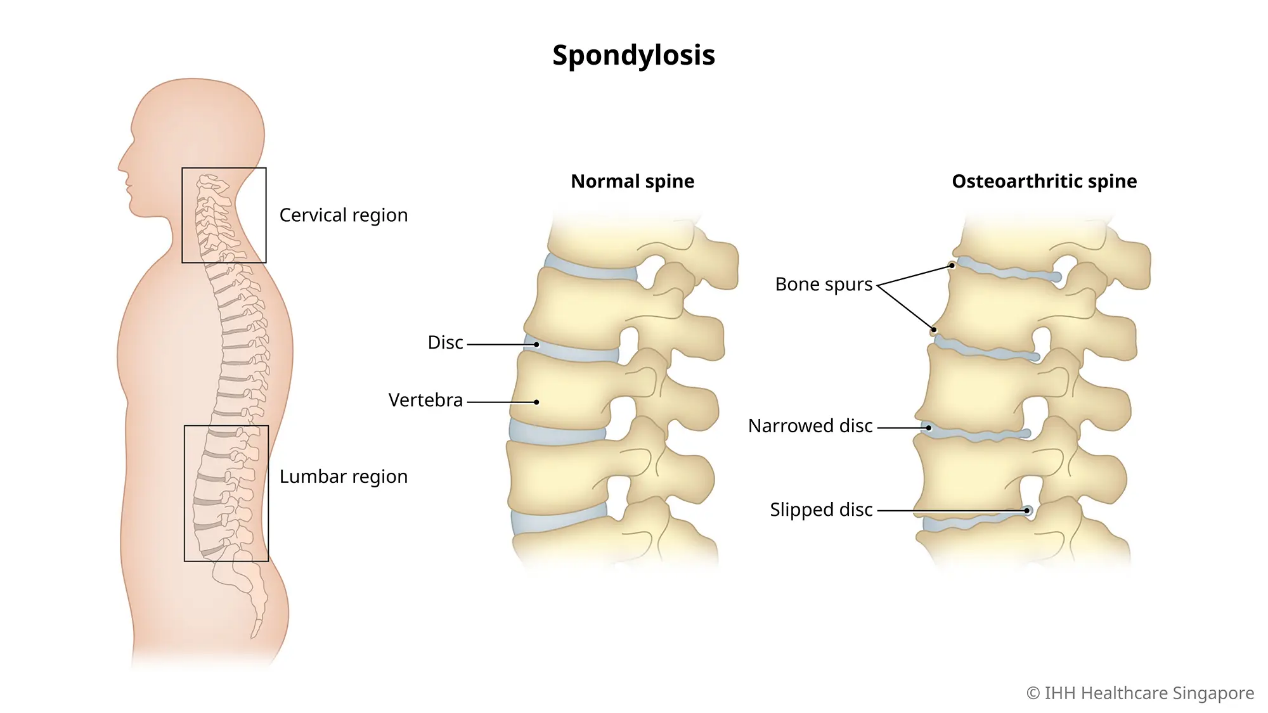
Despite the peculiar name it’s given, Spondylosis is simply osteoarthritis in the spine or what can also be called “normal aging changes.” This is a relatively common diagnosis, especially in the neck and low back. Because this is an age-related phenomena, spondylosis is much more common in older individuals, with up to 80% of adults over 40 having the diagnosis. However, you can have the diagnosis at a much earlier age as well.
So what are these so-called “normal aging changes” involved in Spondylosis?
Absolutely all of us have normal wear-and-tear in our joints as we age and the spine is no different. These changes include degeneration of the disc, or “cushions,” between the vertebrae which can eventually lead to boney changes of the vertebral bodies. There are many contributing factors as to when you may have this diagnosis including your lifestyle, posture, and even genetic/hereditary components. Typically, this diagnosis is given after X-rays are taken and the individual has started having pain in their neck or low back, as well as reduced range of motion. The most common type of spondylosis is in the cervical spine, or neck, and the second most common is in the lumbar spine, or low back.
How can Physical Therapy help to treat Spondylosis?
A Doctor of Physical Therapy can address your Spondylosis diagnosis in various ways. Manual therapy, prescribed strengthening and stretching exercises can help you to regain as much range of motion as possible, as well as decrease the stress on the joints. Physical Therapy can also help you achieve optimal posture and lifestyle changes that will help to decrease the progression of Spondylosis and keep you pain-free for as long as possible.
Now.. what are spondylolysis and spondylolisthesis?
Despite the nuanced difference in spelling, these are very different pathologies from Spondylosis. Spondylolysis is a fracture in the portion of the back of the spine called the “pars interarticularis.” When this type of fracture occurs on both sides of the spine, the affected vertebrae can potentially slip forward in position in the spine. If this forward slippage occurs then the condition is called Spondylolisthesis. It is important to understand the difference in these terms and that if you are diagnosed with Spondylosis, you DO NOT have a fracture, but rather arthritis and some degenerative changes.
Google trend terms: lumbar spondylosis, cervical spondylosis, mild spondylosis, mild lumbar spondylosis, spondylosis vs spondylolysis vs spondylolisthesis, thoracolumbar spondylosis
Other
COMMENTS: No Comments
